Dry Mouth Remedies (Xerostomia)
26 Aug 2015
Dry mouth, or xerostomia, is a common side effect of many medications. It can also be a side effect of cancer treatments, or the result of certain auto-immune diseases. Dr. Sunil Talasila and our team at Talasila Dental Hospital will tell you that for most people, discontinuing their medication isn’t an option.
The solution is two-fold: find ways to increase saliva production and eliminate specific things that are likely to increase dryness in the mouth.
Lack of saliva creates a situation in the mouth that allows harmful organisms such as yeast and bacteria to thrive. It may also make it difficult to swallow food, create a burning feeling in your mouth, or cause bad breath, decayed teeth,among other problems.
Medications that are known to cause dry mouth include:
- Anti-depressant drugs
- Anti-anxiety medications
- Drugs for lowering blood pressure
- Allergy and cold medications — antihistamines and decongestants
- Chemotherapy drugs
- Medications to alleviate pain
- Drugs used in the treatment of Parkinson’s disease
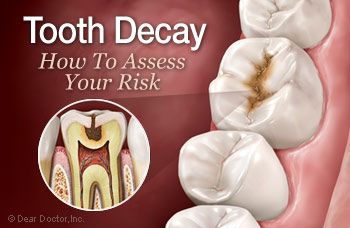
Saliva helps people digest their food. It also functions as a natural mouth cleanser. Xerostomia increases the risk you will develop gum disease or suffer from tooth decay.
Solutions for dry mouth
- Carry water wherever you go, and make a point of taking regular sips.
- Avoid oral rinses that contain alcohol or peroxide.
- Chew sugarless gum or suck on sugarless hard candies that contain xylitol.
- Limit your consumption of caffeine, carbonated beverages (including seltzer and sparkling waters), and alcoholic beverages.
- Brush your teeth at least twice a day, and use dental floss or other inter-dental products to remove food particles that get stuck between your teeth.
- Look for oral rinses and other oral hygiene products that bear the Recognized Dental Association Seal of Approval.
- Brush your teeth and use oral rinses that contain xylitol. Certain gels and oral sprays are equally helpful. Biotene is one over-the-counter brand that makes products designed to treat dry mouth.
- Make sure you get your teeth checked and cleaned twice a year. Dr.Sunil Talasila will be able to examine your mouth for problems and treat them before they turn into something more serious.
You may not be able to solve your dry mouth problem altogether, but you’ll be able to deal with it by following these recommendations. You’ll be able to increase saliva production while reducing your risk of more serious dental problems. To learn more about preventing dry mouth, or to schedule an appointment with Dr. Sunil Talasila, please visit our website http://talasiladentalhospital.com/ for more details.